SURVEY: ILLEGAL DRUGS
Better ways
Jul 26th 2001
From The Economist print edition
If enforcement doesn't work, what are the alternatives?
IMPRISONMENT is unlikely to clinch the war against drugs. What
other weapons are there? Education for the young is one
possibility, although its record is discouraging: one recent report
complains that “large amounts of public funds...continue to be
allocated to prevention activities whose effectiveness is unknown
or known to be limited.” However, for habitual users, the
alternatives are more promising. Drug reformers advocate projects
collectively known as “harm reduction”: methadone programmes,
needle-exchange centres, prescription heroin.
One of the most
remarkable projects
designed to reduce harm
is going on in a clinic two
floors up in a side street
in Bern, in Switzerland.
The clinic is tidy: no
sign, apart from covered
bins full of spent
syringes, of the 160
patients who come two
or three times a day to
receive and use
pharmaceutical heroin.
This Swiss project grew
out of desperation: an
experiment in the late
1980s to allow heroin use
in designated sites in
public parks went badly
wrong. Bern had its own
disagreeable version of
Zurich's more notorious
heroin mecca, Platzspitz.
In 1994 the city
authorities in Zurich and
Bern opened “heroin maintenance” clinics, of which Bern's KODA
clinic is one.
It takes addicts from the bottom of the heap. By law, patients
must not only be local residents: they must be the addicts with
the greatest problems. Christoph Buerki, the young doctor in
charge, describes the typical patient as a 33-year-old man who
has been on heroin for 13 years and made ten previous efforts to
stop. Half his patients have been in psychiatric hospitals, nearly
half have attempted suicide, many suffer from severe depression.
Given such difficult raw material, the clinic has been remarkably
successful.
First of all, relatively few drop out of the programme, in contrast
to most other drug-treatment schemes. After a year, 76% are still
taking part; after 18 months, 69%. Of those who drop out,
two-thirds move on either to methadone, a widely used heroin
substitute, or to abstinence. Two-thirds of the patients, stabilised
on a regular daily heroin dose, find a job either in the open market
or in state-subsidised schemes. Crime has dropped sharply. “To
organise SFr100-200 ($57-113) a day of heroin, you need either
prostitution or crime, especially drug-dealing,” says Dr Buerki. Yet
a study that checked local police registers for mentions of
patients' names found a fall of 60% in contacts with the police
after the addicts started coming to the clinic. Hardly any patients
attempt suicide or contract HIV, because the clinic sees them
daily, monitors their physical and psychological health, and
administers other medicines when they come in for their heroin.
Interestingly, one side benefit of the programme seems to be to
reduce the use of cocaine. Dr Buerki dislikes the idea of prescribing
that drug because of its unpredictable effects. The vast majority
of his patients are taking it when they first arrive, 56%
occasionally and 29% daily. After 18 months of treatment, 41%
have stopped using cocaine and 52% use it only occasionally.
Given that there is no equivalent of methadone to wean cocaine
users off their drug, that is a hopeful finding.
Switzerland's experience, says Robert
Haemmig, medical director of Bern's
Integrated Drug Services Programme,
suggests that abstinence may not be the
right goal for heroin addicts. People can
tolerate regular doses of heroin for long
periods, but if they give up for a period
and then start again they run a big risk of overdosing. “It's always
hard to tell politicians that abstinence is quite a risky thing for
these people,” he says.
Heroin maintenance is still used sparingly in Switzerland, for about
1,000 of the country's estimated 33,000 heroin addicts. Most of
those in treatment get not heroin but methadone. But the
programme's success suggests that there are ways to help even
the most “chaotic” drug users, if governments are willing to be
open-minded. Predictably, the Swiss doubt whether it would work
everywhere: “You need a society with well-paid professionals and
a low rate of corruption in the medical profession,” says Thomas
Zeltner, the senior official in the federal health ministry. But the
economics of the programme are impressive. It costs much the
same as methadone maintenance, and considerably less than a
therapeutic community or in-patient detoxification. It reaches
patients that no other programme can retain. It reduces crime and
legal costs and saves much spending on psychiatric hospitals.
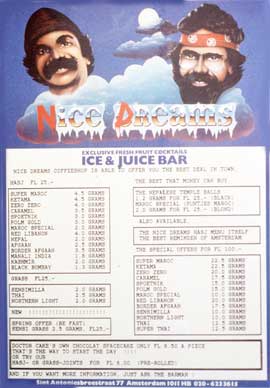
Market separation
The Swiss heroin maintenance programme shows what can be
achieved when a country starts to think of drug addiction as a
public-health problem rather than merely a crime. The Netherlands
has taken a similarly pragmatic approach to marijuana for the past
quarter of a century. It has aimed to separate the markets for
illegal drugs to keep users of “soft” ones away from dealers in the
harder versions, and to avoid marginalising drug users. “We have
hardly a single youngster who has a criminal record just because
of drug offences,” says Mr Keizer, the Dutch health ministry's
drug-policy adviser. “The prevention of marginalisation is the most
important aspect of our policy.”
The Dutch Ministry of Health helps to finance a project by the
independent Trimbos Institute of mental health and addiction, to
test about 2,500-3,000 ecstasy tablets a year for their users.
“When we find substances such as strychnine in the tablets, we
issue a public warning,” says Inge Spruit, head of the institute's
department of monitoring and epidemiology.
What makes this approach work is the Dutch principle of
expediency, which has already proved useful in dealing with other
morally contentious issues such as abortion and euthanasia. The
activity remains illegal, but under certain conditions the public
prosecutor undertakes not to act. Amsterdam's famous coffee
shops, with their haze of fragrant smoke, are tolerated provided
they sell no hard drugs, do not sell to under-18s, create no public
nuisance, have no more than 500 grams (18 ounces) of cannabis
on the premises and sell no more than 5 grams at a time.
Erik Bortsman, who runs De Dampkring, one of Amsterdam's largest
coffee shops, grumbles that the police (and, worse, the taxmen)
raid him two or three times a year, weighing the stock, checking
the accounts and examining employees' job contracts. Sounding
like any other manager of a highly regulated business, he
complains that ordinary cafés that stock cocaine behind the
counter get by with no restraints. He points out, too, that it does
not make sense to allow youngsters to buy tobacco and alcohol at
16 but stop them from buying cannabis until they are 18.
But his main grouse is that, although Dutch police allow the
possession of small amounts of drugs for personal use, he is
forbidden to stock more than 500 grams, and his purchases remain
technically illegal. This contradiction is at the heart of Dutch drugs
policy. Ed Leuw, a researcher from the Dutch Ministry of Justice,
believes that a majority of Dutch members of parliament would like
to legalise the whole cannabis trade. Why don't they? Partly
because it would further increase the hordes of tourists from
Germany, Belgium and France that come to take advantage of the
relaxed Dutch approach; but mainly because the Dutch have
signed the United Nations convention of 1988, which prevents
them from legalising the possession of and trade in cannabis.
However, Switzerland may have found a way around that
obstacle. In a measure that must still pass through parliament, the
government proposes allowing the growing of, trade in and
purchase of marijuana, on condition that it is sold only to Swiss
citizens and that every scrap is accounted for. All these activities
would remain technically illegal, but with formal exemption from
prosecution, in line with Dutch practice. There is no precedent for
this in federal Swiss law. “We wouldn't have done things this way
if we hadn't signed the UN convention,” admits Dr Zeltner.
Extending the model
Could Dutch and Swiss pragmatism be the basis of wiser policies
across the Atlantic? Among lobbyists, the idea that the aim of
policy should be to reduce harm is extremely popular. At the start
of June, the Lindesmith Centre, newly merged with the Drug Policy
Foundation, another campaigning group, held a conference in
Albuquerque, New Mexico, where speaker after speaker argued
that current American policies did more harm than good.
A brave minority of politicians agrees, including Gary Johnson, New
Mexico's Republican governor. He is aghast at the lopsided severity
of drugs laws. “Our goals should be the reduction of death,
disease and crime,” he says, claiming that many other governors
share his views.
For the moment, Mr Johnson is seen as a maverick. “The
harm-reduction approach doesn't sell well in the United States,”
says John Carnevale, formerly of the Office of National Drug
Control Policy. What is forcing more debate, he reckons, is a
movement among the states to allow the medical use of marijuana,
and perhaps the perceived injustice of imprisoning so many young
black men.
The campaign to allow the use of marijuana for medical treatment
recently received a setback with a ruling by the Supreme Court
against the cannabis buyers' co-operatives that have flourished
mainly in California. But public opinion seems to be cautiously on
board: a 1999 Gallup poll found 73% of Americans in favour of
“making marijuana legally available for doctors to prescribe in order
to reduce pain and suffering.”
Change, if it comes, will start at state level. But it will come
slowly. Governments everywhere find it hard to liberalise their
approach to drugs, and not just because of the UN convention:
any politician who advocates more liberal drugs laws risks being
caricatured as favouring drug-taking. Still, the same dilemma once
held for loosening curbs on divorce, abortion and homosexuality,
on all of which the law and public opinion have shifted.
Public opinion is clearly shifting on drugs, too. When the Runciman
Report in Britain last year advocated a modest relaxation of the
laws on marijuana, the Labour government raced to condemn it. It
hastily changed its tune when most newspapers praised the
report. And it is worth recalling that at the time of America's 1928
election, Prohibition enjoyed solid support; four years later the
mood had swung to overwhelming rejection.